
What Are Varicose Veins: Definition of the Disease
The first case of varicose veins was documented in 86 BC. BC: Roman general Gaius Marius complained of pain in his legs from "bruised veins. "
ICD-10 Varicose Vein Codes
- I83. 0 - Varicose veins of lower limbs accompanied by ulcers;
- I83. 1 - Varicose veins of lower limbs with inflammation;
- I83. 2 - Varicose veins of the lower limbs, with ulceration and inflammation.
- I85. 0 - Esophageal varices with bleeding;
- I85. 9 - Esophageal varices without bleeding.
- I86. 0 - Sublingual varicose veins;
- I86. 1 - Varicose veins of the scrotum (anatomy of the male - container of the testicles and their appendages);
- I86. 2 - Pelvic varicose veins;
- I86. 3 - Varicose veins of the vulva (female external genitalia);
- I86. 4 - Gastric varices.
The mechanism of varicose veins
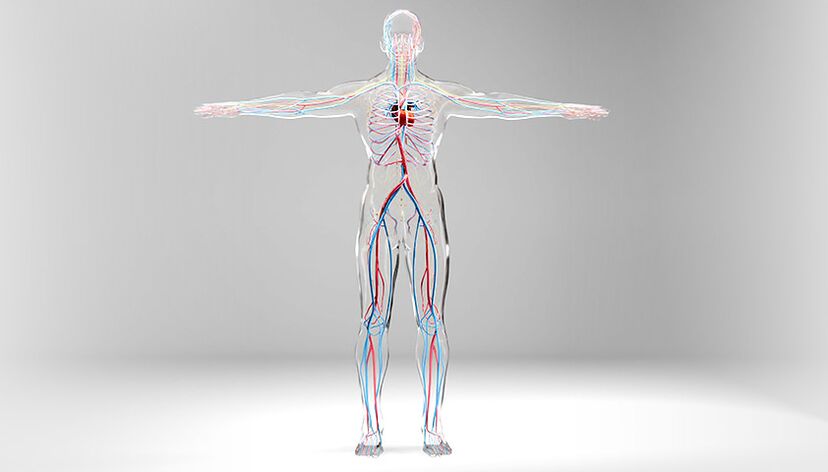
How blood flows in the body
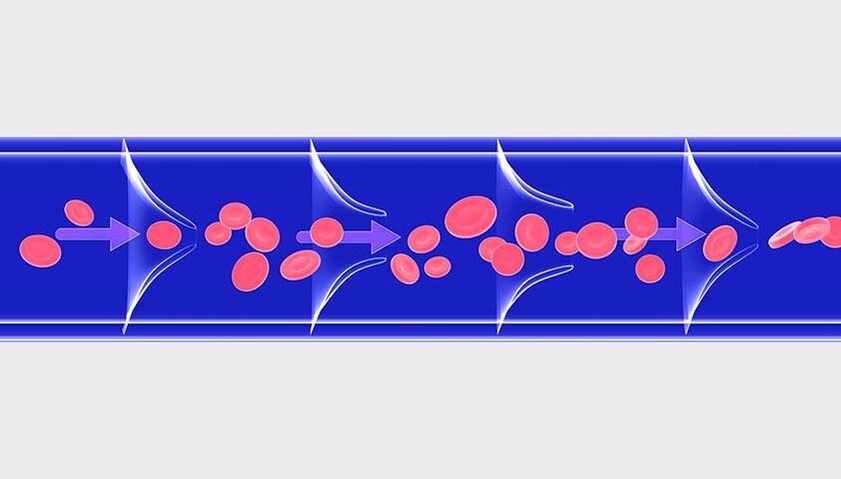
How failure and disease occur

causes of varicose veins
- Lack of physical activity - When you exercise, your muscles stimulate blood flow in your veins, and without exercise, blood circulation in your veins may be difficult;
- Smoking - The chemicals in tobacco smoke can damage the walls of blood vessels, causing the lumen of the blood vessels to narrow and blood flow to become difficult and stagnant, leading to varicose veins;
- Occupations that require standing or sitting for long periods of time - hairdressers, surgeons, chefs, waiters, drivers, office workers are all at risk;
- Menopause - In women aged 40-50 years, the production of sex hormones (estrogen and progesterone) decreases, along with a decrease in the tone of the vein walls. This increases the likelihood of varicose veins.

- Cirrhosis
- liver cancer
- Other conditions that cause increased pressure in the portal system - which collects blood from the abdominal organs
Varicose veins in the scrotum (varicocele)Pathological dilation of testicular pampiniform plexus veins. Presents with scrotal varicose veins and impaired blood flow
- Congenital testicular venous valve insufficiency (usually left side)
- Mechanical compression of the testicular veins (inguinal hernia)
reason:
- polycystic ovary syndrome
- two or more pregnancies
- hormonal imbalance
- Uterine compression of retroperitoneal vessels during pregnancy
- important physical activity
- Uterine and ovarian tumors
Asymptomatic injury to the sublingual vein. Symptoms include slight protrusion of blood vessels and color change from dark blue to purple
- hypertension
- smoking
- old age
- Cirrhosis
- Portal Hypertension Syndrome - Other gastrointestinal disorders (tumors, thrombosis, venous dysplasia) cause increased pressure in the portal venous system
Symptoms of varicose veins
- Fatigue, soreness or heaviness in the legs - this is caused by stagnant blood and the pressure it puts on surrounding tissues;
- Burning, stinging or throbbing in the legs - a reaction to slowing and overflow of blood in the venous system of the lower limbs;
- Nocturnal muscle cramps in the legs - painful cramps that occur due to stagnation of blood and accumulation of metabolic products in the tissues;
- Swelling of the feet and ankles - due to venous stasis, the fluid portion of the blood leaking into the subcutaneous tissue through altered vessel walls;
- Itchy skin around damaged veins - dilated and altered blood vessels are unable to provide normal blood circulation and nutrients to the skin, so the skin dries out and becomes rough.
People with varicose veins experience discomfort in their legs that worsens at night, especially after sitting or standing for long periods of time.

Classification of venous diseases
- C - clinical (clinical changes);
- E - etiology (origin of disease);
- A - Anatomy (anatomical location of varicose veins);
- P - Pathogenesis (mechanism of venous blood flow disturbance).
Complications of varicose veins in the legs


Diagnosis of varicose veins in the legs
Treatment of varicose veins in legs
non-invasive treatment

- Reduction in the manifestations of symptoms - heaviness, leg fatigue, night cramps, burning or soreness;
- The severity of edema is reduced due to improved blood circulation;
- Since elastic compression improves blood circulation and tissue nutrition, it accelerates the healing of trophic ulcers.
- Vascular protectant: improves microcirculation, normalizes increased capillary permeability, and reduces blood viscosity and the possibility of blood clots;
- Antithrombotic agents: Reduce the risk of the formation of dangerous blood clots (thrombosis) in the lumen of blood vessels and promote the dissolution of existing clots;
- Bioflavonoids: Natural plant compounds that improve venous tone and reduce venous congestion.
- Moderate intensity exercise: walking, swimming, water aerobics, leg exercises, yoga. Strengthening the muscles will help normalize blood circulation within the vessels and relieve venous stagnation and edema;
- Weight control: Due to normalization of body weight, the load on blood vessels is reduced, which facilitates the return of blood to the heart through veins;
- Break bad habits: Nicotine and alcohol can damage the lining of blood vessels and disrupt the regulation of blood vessel tone. Quitting smoking and drinking alcohol can improve vein condition and valve function.
Invasive methods of treating varicose veins

With EVLO, the vein is briefly exposed to high temperatures; with RFO, the temperature is lower but lasts longer. Both procedures are effective and safe.
- Venous occlusion using cyanoacrylate glue;
- Mechanochemical elimination, in which mechanical and chemical effects on the container occur simultaneously.
Prevent varicose veins in legs

- Moderate physical activity (walking, swimming, leg exercises) and resting with your legs elevated can improve the free flow of blood through your blood vessels and help avoid venous stagnation;
- Proper nutrition and normalization of body weight strengthen blood vessels;
- Wearing loose-fitting clothing that does not restrict movement can help improve circulation;
- Taking a cool bath during the warm season can help keep your blood vessels healthy;
- Comfortable low-heeled shoes (no more than 3 cm) avoid undue loading on the feet and interruption of blood flow;
- Proper sauna and steam bathing can help you maintain normal blood flow (long-term heat therapy greatly dilates veins, so blood flow slows).























